tv [untitled] November 5, 2012 1:00am-1:30am PST
1:00 am
and move in closer. don't be afraid. the closer you get the more dry chemical powder you will put on the fire and it will go out faster. stay low. before you enter a room feel the door with the back of your hand. if it's hot and you don't see smoke, open it slowly, take a look inside, you know if it's a small fire and you can put it out, do it. work in pairs. the second person is your back up. if the fire is too big, close the door and get help. have 2 emergency exits if you can. there is a fire escape there and the stairway we came up, there's your 2 exists. you seen these before? the hose cabinets. there is a fire extinguisher in there, 50 feet of hose. a nozzle and water in there you can turn it on.
1:01 am
don't do what he's doing. if you turn this on you will have a pile of spaghetti with hose. one person take the hose out to where you are going to put the fire out. tonight open the door, yet and have the other person turn the water on. if you don't feel comfortable, get out. keep yourself safe. we have gauze. this is made of cotton. what class of fire is that? a. >> we have some fire. we have air. we have heat. we have a fire going. if i went in like that what did i just do? >> smoth erred it. simple; right . remember the hot water heater,
1:02 am
we say don't store gasoline in your garage? so, gasoline gives out vapors, if we heat this up. not that you have to heat the gasoline. if you store gasoline near a hot water heater the vapors alone will catch fire. the vapors travel and caught. you don't have to actually light something like a candle, you don't actually have to touch something. we will add, more, make more effect, here. you got cherries jubilee. how do you put this out? [laughter]. put the lid? what if you don't have a lid? cookie sheet. >> very good.
1:03 am
that's a good one. cover the thing, take it off the burner. take it off. do i immediately open it again? no. you already put it out leave it alone and whether or not it is the cheapest fire extinguisher you can buy? baking soda. have a couple boxes of baking soda, near the stove. cut the top off so it's ready to go. you get the box and, boom, dump it on there. you don't stir is around. you smoth erred it, baking soda doesn't burn. now, we are down to the home work. read these pages in your book, 26-38. locate the gas, water, electric
1:04 am
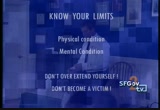
shut off inside and outside the home. do the course evaluation. crank the gas an eighth of a turn to make sure it works and you know where it's at. very good. thank you. [applause]. there are three things we want you to take away. how to open a air way and when to do it and control bleeding and treat shock and we want to talk about disaster medicine an death by trauma and by that i
1:05 am
mean the body is acted upon by outside force and first is instant yainous and occurs in minutes and are we going to do much for this person? not so much. maybe in the predisaster situation and making the place safer but once someone is hit with something heavy and die within minutes you're not going to happen, and the next is occurring within minutes of the injury and bleeding to death or having their air way blocked or some unrecognized medical problem and this is the group we're going to help, and the third is die afterwards from infectionsoir things that go wrong with the recovery process. we can help by delivering prope first aid and keeping things
1:06 am
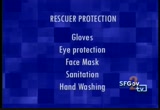
clean but this isn't the target group and these are the people to be aware of, in the middle and people are talking about blood and this brings up the concept of res curer protection. gloves, eye protection, and masks and sanitation and hand washing and who among us don't have a nick or a cut on their hand and are you going to touch someone's blood and your in tac skin will protect you from most ilknows. however, if you have a cut on your hand you have a path for infection to get inside of you and you want a pair of latex gloves -- several pairs of glo gloves that you can put on and change as you go from patient t patient hopefully and at least
1:07 am
wash your hands and disinfect your hands between patient contacts and the eyes are like an open wound and path to get into your body and glasses and take the old glasses and throw them in your kit and you have something to wear and face mask and of course dust and dirt and all of these disasters throw up dust and dirt and especially in a dryer season and push comes t shove a band da bandana. and after a disaster is not the time to let your hygiene slip and it's a time to tighten it u
1:08 am
and communitycable diseases and if it's wet and not yours don't touch it. gloves and every patient contac and don't touch blood and it's good rule to live by. hepatitis a and sal min nillia and geria and assumed to be in the fresh water in california and you get enough of the parasites in you and you will b in the bathroom for weeks and you won't be happy about it and make sure you have clean water stored in your disaster kit and be aware of the source of the water and hepatitis a and wash your hands. salminila and is it safe and
1:09 am
should i be eating this and not properly prepared and know wher the food comes from. tetni and disease -- oh you stepped on a rusty nail and it' not exclusively rusty nails and you have a cut and open wound and at the timeu at the time dm here and these are the first things you check for in any patient you see. if they don't have an air way they can't breathe and then wha are they? >> (inaudible). >> dead and we will review that and it's a basic point. okay. if you are plea are bleeding an
1:10 am
important to keep in mind that most bleeding stops on its own and all bleeding stops essentialls shrcials eventuaeve. medical joke and if you are in shock -- and no hurt nerves we don't want you to go in and hel somebody and have something fal on you and get other hur hurt. look, listen and feel and have you ever put your chin to your chest and it's tougher to breathe and tilt your head back and easier to get a breath and we tilt the head back, lift the jaw up off of the air way and i opens the air way. this young lady is in the classic position and take first
1:11 am
aid and take cpr class and ther is any and she'y annie and she' and in a disaster you don't fin people in this position and sometimes i walk up and i can't tell whether they are breathing or not and you have to get closer and you have to touch th person and shake and shout "are you all right? " and no response and then you touch annie and shake her and n response, and what you do is pu the person in a neutral positi position, on the back so you ca open the air way if you think they're not breathing. if they are breathing and you shake annie and she says "go away, i'm sleeping here" you
1:12 am
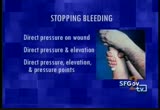
don't have to move her. how much blood do you have? about 6-liters and how much of the red fluid would it take to soak the front of my shirt? not much and one of the little lobes in the bottom here, half an ounce would coat my shirt an if i were to take this and pore it out on the wooden flee floor make a mess and all over the place and difficult to gi gauge blood loss by what you are looking at and there is an emotional component to it and this is a lot of blood and ble bleeding control and pressure and elevation and pressure poi point. to stop bleeding you put direct pressure on the wound. then you do direct pressure and elevation and then you do direc pressure and elevation and a
1:13 am
pressure point. direct pressure on the wound an dressing goes on it and a bandage holding it in place. oh my gosh the dress acknowledges soaked through and what do i do? take it off and throw it away? no. put another one on top and hold tighter and get a good grip on it and if you elevate the affe affected part it will redhiew r blood pressure and headach make harder for the blood to come ou and we will talk about pressure points in the body and in the upper arm here and this around the pelvis and you can practice this one at home with a friend and we will do this one here. okay. take your left arm and hold it up, 90-degrees here and take th four fingers of the hand and yo find a muscle on top and muscle
1:14 am
below and in the middle there i a bone and you feel on the bone with the forefingers and somewhere in there you will fin a pulse and you mush it up against the bone and if somebod was taking your pulse at your wrist this time the pulse would disappear. what you're doing is reducing the flow of blood to the affec affected part, to the arm. okay. what you're not doing is blocking the venus return. you're not sequestering blood the affected part and not blocking it off entirely. if you blocked it off entirely what is that called? a turn kit and we try not to us the t word in disaster medicine
1:15 am
and tiewrn kits are -- turn kit are too often used by the publi and elevate the pressure point before you think about that. what is this patient suffering from? >> (inaudible) a little bit too much maker up an make up and we shock. and there is little phrase here comfort and reassurance and victims don't care what you kn know. they just want to know that you care. i am going to be busy. and doctors and emergency personnel are busy and they don't have time to comfortable people, and lives can be saved by the vej len vigilence of unt
1:16 am
personnel and you are there wit a family member and sit with a person and pat a hand, and mop fevered bra and these are important things that volunteer can do. shock. what is shock? it's the inadequate profusion o the body's cells that can lead to not enough oxygen in the brain and the brain needs two things to work. oxygen and sugar and if you run out of one the brain cells begi to die and if blood is not getting up there you're not getting either one of those. how many of you have seen someone faint? they get bad news or cut their foot and did you need a doctor to tell you there is something wrong with the person? and you don't need to be a pro- and when someone is facing that
1:17 am
shock and facin face fainting i way of telling you to lie down and signs and symptoms of shock confusion. disoriented, unconscious and skin pale and moist and pulse rapid and you have a problem here and you are nausea and thirsty or you can be thirsty and then nausea and here is a bottle of water and then they get nausea and they throw up an they're having trouble and they go unconscious and throw up. not so good. people die that way. the rule is nothing by mouth in the prehospital field and nothing by mouth and the treatment for shock is
1:18 am
remarkably simple. lay them down and raise the fee about a foot and keep them warm and they're chilly and the brai doesn't feel it and they will feel cold and you want to keep them warm. your patient is never shiver an first thing is always seeing safety and don't go rushing in and be cautious when you approach them. norm, are you all right? if i can't tell he is breathing and i get closer and norm, are you all right? give him a shake. are you okay? if there is no response then yo have to look, wait a minute is he breathing? if he has a filing cabinet on
1:19 am
top of him or covered with debris and maybe you can pull some of it away and evaluate hi breathing and put him in a tru traneutral position and neck injuries are rare and they are very dangerous but very rare an besides if you're not breathing what are you? >> (inaudible). >> so what you do is move them gently, and we're not trained and what you do is move them gently and using common sense a individual and role on back and look, listen and feel and not breathing and i better open his air way and push down on the forehead and notch under here and you lift up and this will open the air way. now, this position and especially on a flat surface is
1:20 am
a little uncomfortable and he's not going to stay in this position, so since you're nert people and you always work in teams and you always have your manual with you and two or thre manuals and slide them under hi shoulders, or you could take a shoe off and put it under the shoulders and make its so the head flops back a little bit an keeps the air way open and whil you attend to this and he's bleeding and not breathing and now he's bleeding. so direct pressure. still bleeding -- put another dressing on and you can hold it in place with a bandage and if he wakes up hold on to this or you're going to die.
1:21 am
he tends to hold on nice and tight and it's still bleeding. well, let's find this pulse point in here and we will push against the bone there and it will slow the blood and it's al good and bleeding stopped and hold on to that for a while and make sure the bleeding doesn't reoccur, and this guy ought toe a doctor and it's real bad and in fact we can tell him to see doctor and he has sweat and be beading up on the forehead and looking pale and what do we do for someone who is pale and not responding well? what you want to do is raise hi feet about a foot and you can get creative about how you do i and you need something under th feet and take a chair on its side or take the shoes off and
1:22 am
under there and take the bags lies around here and stick it under the legs and so the blood will flow out of the legs and t the mush where he needs it. >> okay. now that you know how to treat patients and what i am going to talk about is something called triage and it's going to tell you who to treat and we're goin to sort patients and when you sort patients and one of the things people don't understand and it's different than treatin patients and you have to trea t them first and you know what yo have and then you can treat the with what you learned in the first half with steve and the goal of triage happens to be th motto of nert "do the most good for the most people" and if there is an earthquake right no and ceiling collapsed and 40
1:23 am
people in here, and if i'm the one rescuer coming to you and the first person is not breathing and no pulse, would you want me to stop and do cpr for this person before i reache you and what if there are 500 people behind that and do cpr and i just have to open an air way and all patients fall unde under -- and i'm going to use colors and green, walking wounded and anybody that walks. d for delayed or yellow meaning you're hurt but you're not hurt enough. you're not hurt but that no not that bad an.
1:24 am
and d is dead. and dead is the easiest one to determine. and how do we determine whether someone is dead? they're not breathing, right an steve said that several times and how do we know someone is not breathing? we look, listen, and feel and open the air way and we look to see if the chest is rising and listen to feel air and how long do we check for actually? american red cross o says about ten seconds and if they are not breathing we readjust the air way and check for ten seconds again and not breathing for the secretarsecond time we said say and you check the air ways twic
1:25 am
and when you know someone is dead you move on. let's go through the categories. walking wounded and anybody tha follows directions and get up and walk and it's green. d is delayed and anybody that i injured but we don't think it's life-threatening. i is the people that need treatment right now and d is th dead and black and during triag you open an air way and how lon does that take? two seconds and it takes ten seconds to check and bleeding - the only bleeding i want you to treat during triage are arteria bleeding and spurting out and you could bleed to death in about three minutes and shock and if the person is unconsciou
1:26 am
on the chair and how do i treat for shock? lay down and lift the feet and cover you and takes ten -15 seconds and i move on. the categories, black for peopl that are dead and green people that are walking and the only two categories left are red and yellow. this rule here that i'm going t teach you now and i want you to memorize it and this is the rul that is going to determine whether you're red or you're yellow. the rule is 32 can do. i want everybody to say it with me. thirty-two can do. it's a three part rule. thirty, first part and 30 is respiration and it's the amount respirations per minute and if someone is breathing faster tha 30 times per minutes and it's
1:27 am
about a breath every two second and if i breathe like this. that's about faster than 30 right? and if you have a patient breathing 30 seconds and they fail and tag them red and you move on. if someone is breathing normal than you go to the next rule. they pass and if go to the next rule. thirty-two is blood -- also ca called capillary refill and the blarch test and capillary refil and look ata palm of your hand or fingertips and the nail beds are usually pink and if you squeeze and do it on yourself right now and squeeze your finger and it turns right and when you let go the pink return and i hope everybody in the roo
1:28 am
i hope the pink returns in two seconds and if the pink comes back in two seconds you pass an if it takes longer you fail and you tag red and move on to the next patient and we have two rules. thirty and breathing faster and they fail and blarch test faste than two seconds and fail and can do and if someone can follo simple commands. look at me. tell me your name. give me your hand. and if they can follow simple commands they pass. if i say "look at me" and they're not looking at me and "tell me your name" and they don't do anything "give me your hand" and they do something else they fail and tag them red and to the next patient and thi
1:29 am
is the one of the hardest thing to grasp is how to triage and green, anybody that walks and blad and dead an -- dead and bl twice and red if you fail and either of the three parts of th rule. thirty-two can do. we're going to try this right now. okay we will stop here because think we get the point. who are the first patients you came into contact with? and you were tagged yellow. and you tagged yellow because?
71 Views
IN COLLECTIONS
SFGTV2: San Francisco Government Television Television Archive
Television Archive  Television Archive News Search Service
Television Archive News Search Service 
Uploaded by TV Archive on

 Live Music Archive
Live Music Archive Librivox Free Audio
Librivox Free Audio Metropolitan Museum
Metropolitan Museum Cleveland Museum of Art
Cleveland Museum of Art Internet Arcade
Internet Arcade Console Living Room
Console Living Room Books to Borrow
Books to Borrow Open Library
Open Library TV News
TV News Understanding 9/11
Understanding 9/11